I’ve been following the medical-ethics debate on setting priorities for Covid-19 vaccinations, and thought I had a good handle on it, when I read this provocative comment in the Senior News from Julie Fulkerson, ex-mayor of Arcata and much else:
“I could even argue that those who refuse to wear masks should be higher on the list. At least they could get the vaccine and save a lot of others from infection.” Rewarding those who put the rest of us at risk? That sucks—and makes total sense! (That’s assuming a vaccine, in addition to preventing infection, will also stop transmission—currently unproven.)
So how do we figure out who gets the vaccine first…and second, and third? The Center for Disease Control (CDC) lost credibility, in my book, with their late endorsement of masks, delaying their recommendation until April, three months after the virus arrived in this country. Still, the CDC is all we’ve got as far as suggesting a nationwide policy for vaccine priorities, issuing an advisory to states on December 23: “…initial supplies of COVID-19 vaccine [should] be allocated to health care personnel and long-term care facility residents.” The recommendation was in line with the CDC’s threefold goals: to decrease death and serious disease as much as possible; preserve functioning of society; and reduce the extra burden COVID-19 is having on people already facing disparities.
No question, of course, about prioritizing the nation’s 21 million health care personnel. Other than the obvious ethics here—they’re the ones in daily contact with actual or potential Covid carriers—the “put your own oxygen mask on before helping someone else” airplane safety rules apply. Keep the medics healthy so they can take care of us if we get infected!
More controversial is, why are the three million (in the US) long-term care facility residents prioritized? Rather than minimize lives lost, shouldn’t we be trying to save years of life lost? This is Peter Singer’s “utilitarian” argument. (Utilitarianism, you recall, is the theory of morality promoting actions that result in the happiness of the greatest number of people.) Singer is an Australian moral philosopher (now at Princeton) whom I greatly admire—his 1975 book Animal Liberation prompted me to give up eating meat many years ago. In a recent—and fascinating!—discussion printed in The New York Times Magazine on the subject of vaccine priorities, he said, “The objective that we should aim for is to reduce years of life lost. I know a lot of people are talking just about saving lives. But I do think that it’s different whether somebody dies at 90 or 50 or a younger age still.”
The New York Times Magazine article that prompted this column.
So: do you give priority to a 90-year-old with an expected lifespan of 4-5 years, who has a high risk of dying if they contract Covid; or to a 50-year-old, anticipated lifespan 30-33 years, with a low risk of dying if they’re infected? (I’m 78, in excellent health. According to this, I can expect to live another nine-odd years. Why should I get the vaccine ahead of someone in their childbearing years?) Here are more questions for your consideration:
Prison populations: Like elder care facility residents, prisoners are stuck inside in potentially risky environments. Not even potentially: all of California’s 35 state prisons report having Covid, with over 32,000 cases to date. These are people with, on average, much longer projected lifespans than care facility residents—what about giving them priority?
Race and Ethnicity: According to the CDC, Black, Latino and Native Americans are nearly three times as likely to die from Covid infections as white and Asians. Should they be given priority?
Teachers: Along with all front-line workers and those delivering essential services, isn’t vaccinating teachers a no-brainer? Education is critical! Teachers (6.6 million in US public schools) are largely responsible for the next generation—what children know, what they value, what life is about. Plus, of course, we currently have countless parents—who would otherwise be working—taking care of their kids at home.
Rest of the World: Pandemic means worldwide. We’d be really stupid—not to say unethical—if nationalism in this country (and other high income countries) got in the way of immunizing people in the many poorer countries, especially in the Global South (where most of Earth’s young people live). Yet that’s what’s happening: we have dibs on enough vaccines to inoculate our entire population four times over, as does the UK; Canada has lined up six times what’s needed for its population; the European Union twice its population. All at the expense of less fortunate countries. Shouldn’t we be focusing on the whole world, rather than our corner of it?
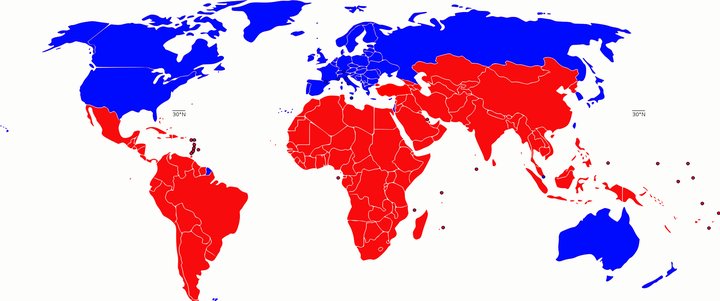
The “Global South”, in red, is replacing the old “Third World” value-laden designation.
These are some of the questions that decision makers are wrestling with. What’s your take?
CLICK TO MANAGE