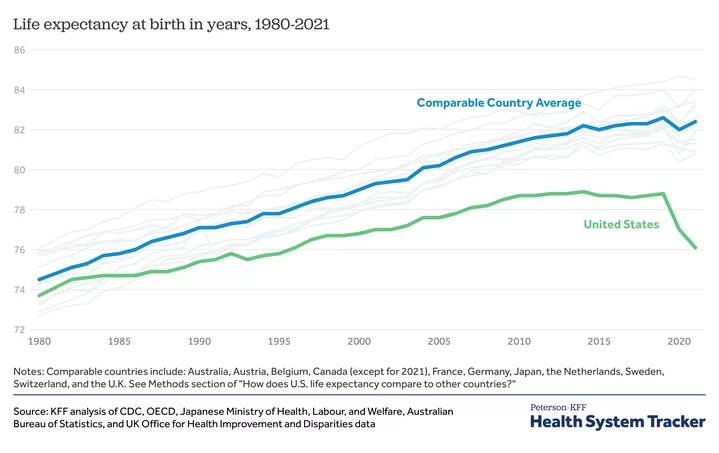
You read that right. I didn’t mistype New Hampshire’s state motto, adopted in 1945 and which probably had its origins in French Revolutionaries’ Vivre Libre ou Mourir. Fact is, our yearning for personal independence and autonomy is probably responsible for a shocking factoid: post-Covid life expectancy, which had decreased in most countries in 2020, bounced back everywhere except in the US. According to the CDC, while U.S. life expectancy at birth dropped nearly three years from 2019 to 2021 (78.8 to 76.1), comparable countries barely registered Covid between the same years (82.6 to 82.4). Here’s a summary of the CDC’s findings, and how it came up with them.
Even without Covid, we’re still doing terribly: We’re far outspending other large, wealthy countries in healthcare, yet we have the lowest life expectancy—also by far. Outspending by how much? “In 2021, the U.S. spent 17.8 percent of gross domestic product on health care, nearly twice as much as the average OECD country,” according to the Commonwealth Fund.
Got that? We spend double what comparable countries spend on healthcare, and live six years less than they do. Not just rich OECD countries, either. “They” in this case includes citizens of Cuba, Lebanon and Czechia (previously Czech Republic), none of which are usually considered part of the “first world.”
Graphic: Peterson-KFF Health System Tracker.
What’s going on?
Ten years ago, a panel of experts convened by the National Academy of Sciences published a report titled “Shorter Lives, Poorer Health,” which accurately predicted our current situation. According to the report, “A big part of the difference between life and death in the U.S. and peer countries is people dying or being killed before age 50.” It specifically points to “factors like teen pregnancy, drug overdoses, HIV, fatal car crashes, injuries, and violence.” Interviewed more recently by NPR, one panel member, Eileen Crimmins, professor of gerontology at USC, has a harsh word for lovers of assault weapons (see last week’s guest column on the Nashville shooting): “Two years difference in life expectancy probably comes from the fact that firearms are so available in the United States.” In addition, “There’s the opioid epidemic, which is clearly ours – that was our drug companies and other countries didn’t have that because those drugs were more controlled.”
One unexpected finding of the NAS panel is that our worse health and shorter lifespan isn’t just confined to poor and minority cohorts, but extends through all sections of society, including the one-percent. Money isn’t always the answer. In fact, economics is a critical part of the equation: Extra health care costs the country “as much as $100 billion annually.”
What’s the answer? A willingness to learn from other countries, instead of going it alone — that is, a dose of humility! — would sure help. And specifically, according to Steven Woolf, director emeritus of the Center on Society and Health at Virginia Commonwealth University (in an interview on NPR) “…universal, better coordinated health care, strong health and safety protections, broad access to education, and more investments to help kids get off to a healthy start. These policies are paying off for [other countries], and could for Americans, too.”
CLICK TO MANAGE