OBITUARY: Lonnie Mack Martin, 1958-2025
LoCO Staff / Friday, Jan. 2 @ 6:56 a.m. / Obits
Lonnie Mack Martin
1958-2025
A life well lived.
It is with deep sorrow and heavy hearts that we announce the passing of our loved one, Lonnie Martin. Our beloved advanced into heaven at home in the loving arms of his soulmate, Kathleen Little, to be with, by grace, our Lord on December 21, 2025, after a month-long battle in the hospital where he fought complications from COPD and RA. Lonnie wasn’t ready to leave us all on Earth quite yet, but his body regrettably had other plans. We were honored to respect his brave wishes of returning home so he could go peacefully where he wanted to be, where his heart was, at home in Rohnerville.
Lonnie was revered as a son, a nephew, a brother, a cousin, a husband and life partner, an uncle, a dedicated and proud father, a grandfather, and a great-grandfather, but most of all, he was our tremendous friend. He was regarded as a gallant man who loved his family the most although he also enjoyed earthly pleasures of buck hunting, country music, drag racing, coaching youth sports, baseball (go, Giants!), western movies, BBQing, gardening, and caring for pets. Lonnie particularly enjoyed ringing the family cowbell in support of all his son James’ regional baseball and all-star games while cheering him on. He also enjoyed going to Maui with his family and soaking in the sun and beauty offered there recently. Losing Lonnie is a stark reminder to hold your loved ones close because every day is a gift, and tomorrow is not promised. The grief felt by his loss is insurmountable.
Lonnie was born in Fresno then raised in Humboldt County from age three, where he eventually attended Fortuna Union High School. In 1964, the Martin family was displaced from Stafford when the floods took the house off its foundation and down the river. They lost most everything but the clothes on their back at that time. After that, the Martin family moved to North Court in Scotia for a few years when Lonnie’s dad worked at the Scotia Mill, and then finally to Fortuna on Garden Lane where Lonnie and his siblings attended South and Town Schools. They enjoyed camping together at the beaches and at Swimmer’s Delight in Carlotta during the summers, and spending time together at the Grange.
Lonnie became skilled at many trades. He was an automotive mechanic and enjoyed building and driving his Firebird 400, Chevy Vega, Cheville, Camaro, and Mustangs. He also spent time working at Halverson’s Sawmill, Carlotta Lumber, and B & J Roofing.
Lonnie had the eyes of an eagle, and a heart of gold. We called him a hummingbird because of his love of all sugary things. He had a wonderful sense of humor, a joking personality, and his way of showing love often involved poking fun at you. We will miss his kind demeanor, joyous laughter, and boisterous and outspoken presence that defined him up until the sudden end of his life. It was a privilege to have known him, stubborn and determined as he was. Underneath his reserved exterior, he maintained a certain tenderness which can only be described as selfless kind-heartedness and empathy towards others. He often found happiness in everyday life through watching the flowers bloom and listening to the birds sing in his backyard and being with, and there for, his soulmate Kathleen. He is sorely missed and was deeply loved and appreciated by all who were blessed enough to be in his presence and called his friend.
Lonnie was preceded in death by his grandparents, Ira Martin, Alice Martin, Mack Williams, and Violet Williams, parents, James Martin and Nina Martin, sister, Deborah Gutierrez, uncle, Wayne Martin, mother and father-in-law, Margaret Philpot and Thomas Philpot, brothers-in-law, Miguel Gutierrez, Robert Philpot and Dennis Philpot, sister-in-law Gloria Philpot, and his grandson, Daniel Hernandez.
He is survived by his soulmate and life partner, Kathleen Little, their cherished children, grandchildren, and great-grandchildren, James (Natalie) Martin, Peyton Martin, Monika (Jesse) Mayhan, Margo Mayhan, Sara Little, Emerald Robinson, Zackariah Spencer, Jeremiah Spencer, Lailoni (Matthew) Farnsworth, Felipe (Makayla) Hernandez, Freya Hernandez, Solinda Hernandez, Elizabeth Hernandez, Jamie (Jason) Wray, Jason (Lani) Wray Jr., Kimika Wray, Nakaila Wray, Leann Martin, Brandi Martin, Sie Arnold, Luci Arnold, Lydia Martin, Wyatt Martin, Kyle (Christa) Martin, Kylee Minica, Ryleigh Callahan, Kaycee Martin, Aaleigh Kerney, aunt Betty Martin, brothers Larry (Shelia) Martin, Loren Martin, nephews and nieces, Miguel (Tiffany) Gutierrez Jr., Ashley Gutierrez, Isaak (Paige) Gutierrez, Larry (Jennifer) Martin, Dustin Martin, Jordan Martin, Gavin Martin, Ira Martin, Mira Martin, Preston Martin, Brooke (Ben) Martin-Gill, Jonathan (Kelly) Philpot, Kailaya Philpot, Thomas Philpot, Jamison Philpot, Regina (Tina) Amaral, Lacey (Cameron) Amaral, Owen Conatser, Angela (Jeremy) Arrington, Victoria Arrington, Allora Arrington, Davina Arrington, Eleanor Arrington, Vanessa (Tom) Herr, Hailee Herr, Aaliyah Herr, David Herr, Alivia Herr, Havana Herr, Roseabella Herr, Melissa (Ritchie) Blake, Logan Blake, Bryce Blake, Amanda Blake, Emily Blake, Becca Blake, cousins, Donald Martin, Walker (Kylie) Martin, Cedar Catanio, Lloyd Nichols, Karen Nichols, James Nichols, Lexi Coleman, Roy Nichols, Jess Nichols, Jeanette (Gary) Trone, Kevin (Krista) Trone, Brandon Trone, Mary Martin-Webb, Stephen Webb, and Chris Webb. He is also survived by numerous other friends and relatives. Special mention of his primary caregiver and friend, Bobbi Reese, for years of not only great friendship, but also excellent and devoted specialized care.
Celebration of life services for Lonnie have been arranged and will be held on Saturday, January 31, at the Veteran’s Hall in Fortuna at 1 p.m. Friends and family are welcome toattend the potluck and share in paying tribute to his accomplishments as well as mourning his loss. Guests are encouraged to bring cherished photos, memories, and a dish to share in his honor. His eternal resting place will be at the Sunrise (Newberg) Cemetery in Fortuna. The family wants to thank friends and relatives for their presence and support during this challenging time, as well as Hospice of Humboldt for their service.
###
The obituary above was submitted by Lonnie Martin’s family. The Lost Coast Outpost runs obituaries of Humboldt County residents at no charge. See guidelines here. Email news@lostcoastoutpost.com.
BOOKED
Yesterday: 4 felonies, 11 misdemeanors, 0 infractions
JUDGED
Humboldt County Superior Court Calendar: Today
CHP REPORTS
1740 Mm96 E Hum R17.40 (HM office): Traffic Hazard
Myrtle Ave / Harrison Ave (HM office): Defective Traffic Signals
ELSEWHERE
RHBB: Wet Winter, Dry Reality? Humboldt Officials Say Water Risk Isn’t Gone
RHBB: College of the Redwoods Del Norte Campus Project Moving Forward with Measure I Funding
RHBB: Major Roadwork Scheduled Friday, February 6 through Thursday, February 12
Fishing the North Coast : Finally — Rain on the Way for North Coast Steelhead Rivers
OBITUARY: Erling Dellabalma, 1939-2025
LoCO Staff / Friday, Jan. 2 @ 6:56 a.m. / Obits
Erling Dellabalma
March 18, 1939 - Dec. 20, 2025
Dad left us unexpectedly on December 20, 2025. He was 86 old.
Dad was born on March 18, 1939 to Natale and Mary Dellabalma of Orick.
In 1944, his parents bought a dairy farm in Elk River, where Dad worked with his father, and brothers, Donald, Raymond, John, and James. He attended St. Bernard’s Elementary School, then went to Eureka Senior High School so he could enroll in the building trades classes. He graduated in 1958.
After graduation, Dad worked as a carpenters apprentice. In 1959, Dad’s parents gave him a plot of land to build a house. Dad married Mom, July 3rd, 1960. A little over a year later, the first of five children was born.
In October of 1961, they moved into the house they had built, and lived there together for over 64 years.
Dad was a loving father, and husband.
Dad worked at three different lumber mills, Vandenor Lumber, Georgia Pacific, and finally at Schmidbauer Lumber , where he started as a loader operator, and later was promoted to timber buyer, and made many friends.
In 1989, Dad and Mom purchased the Sullivan Ranch in Elk River and started a dairy. After several years, the decision was made to sell the dairy cows, and start raising beef. After almost 35 years, Dad retired from Schmidbauer Lumber, and became a full time rancher.
Dad loved making hay.
Dad was very generous, always ready to lend a hand, and a friend to all. It was not uncommon for Dad to run into someone he knew wherever he went. Dad loved family get togethers, his home, ranch, and Christmas.
He was a lifelong member of St. Bernard’s Catholic Church. He was also a member of the Sons of Italy, and Native Sons of the Golden West.
Dad was preceded in death by his parents, Natale and Mary, his brothers, Raymond, John, and James, and his youngest son, Kevin. He is survived by his wife of over 65 years, JoAnn, his daughter Macheal Haskins (Dan) and his sons, Michael, Robert, and Tim. His grandchildren, Sarah, Katie, Matthew, Dylan, Rebekah, Aleksandra , Clarence, Samuel, and Elizabeth. Great-grandchildren, Ella, Abel, Solomon, Noel, Elora , Mathias, Iden, and Elijah.
There will be a rosary at 9:30 a.m., and Mass at 10 a.m., both at St.Bernard’s Catholic Church, in Eureka, on January 14, 2026. In lieu of flowers, please make a charitable contribution to St. Bernard’s Church.
###
The obituary above was submitted by Erling Dellabalma’s family. The Lost Coast Outpost runs obituaries of Humboldt County residents at no charge. See guidelines here. Email news@lostcoastoutpost.com.
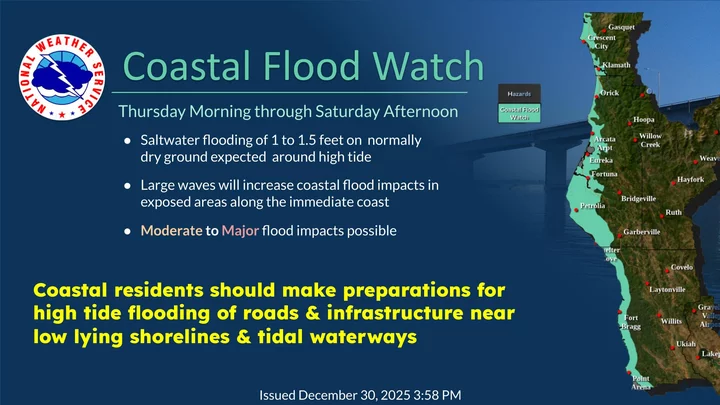
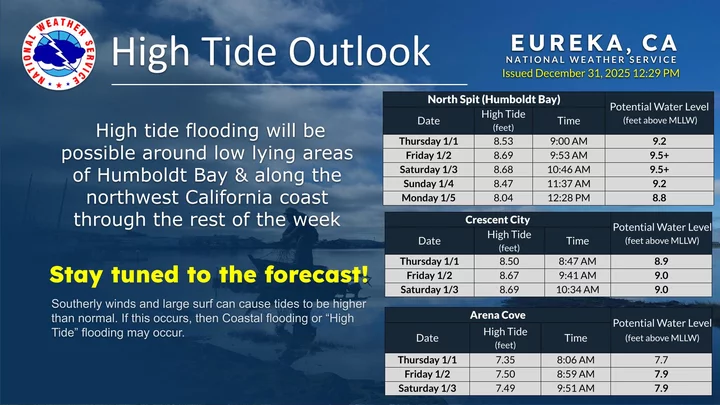
COASTAL FLOOD WATCH: Stormy Weather and King Tides May Cause ‘Moderate to Major’ Flooding Along the North Coast
Isabella Vanderheiden / Wednesday, Dec. 31, 2025 @ 1:36 p.m. / How ‘Bout That Weather
Graphic: Eureka National Weather Service
###
Heads up, coastal dwellers! Over the next few days, an incoming storm and high atmospheric tides will almost certainly cause flooding along low-lying shorelines and flood-prone areas around Humboldt Bay.
A Coastal Flood Watch is in effect Thursday morning through Saturday afternoon.
“A Coastal Flood Watch means that flooding is possible but not imminent,” according to the National Weather Service advisory. “High astronomical tides and large surf may cause moderate to localized major flooding in low-lying areas along the Redwood Coast. Up to 1.5 [feet] of saltwater inundation above ground level is possible in low-lying areas near shorelines and tidal waterways.”
The rain could start up as soon as tonight, but it won’t get stormy till Friday.
###
Graphic: Eureka National Weather Service
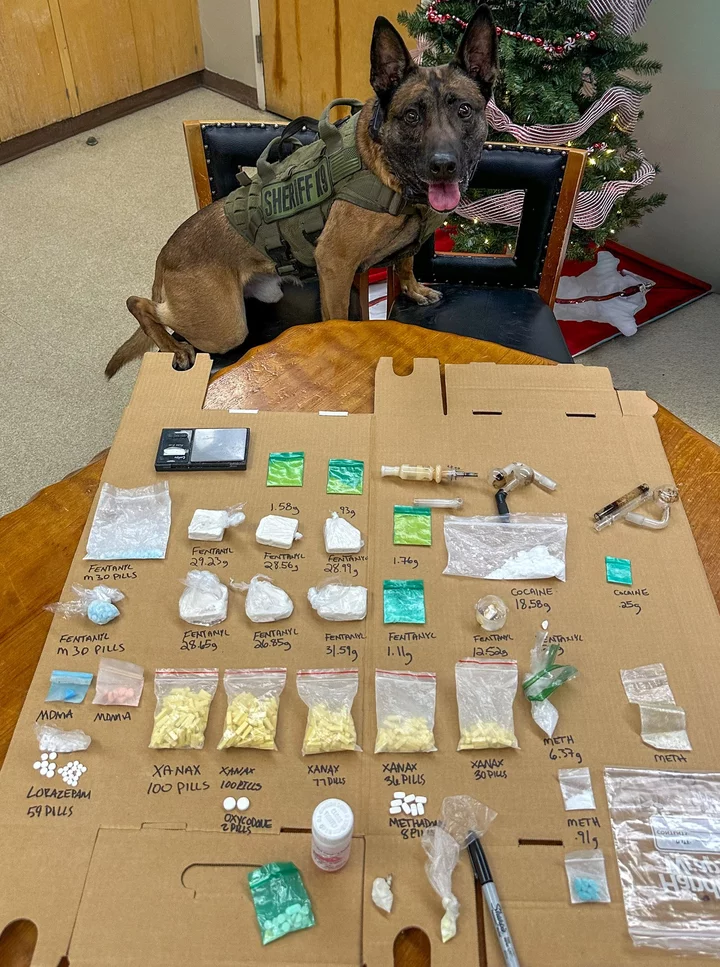
A Sheriff’s Office K-9 Unit Sniffed Out a Massive Collection of Illegal Substances During a Salmon Creek Traffic Stop Yesterday; Two Eel River Valley Residents Arrested
LoCO Staff / Wednesday, Dec. 31, 2025 @ 10:41 a.m. / Crime
This is how K-9 Yahtzee rolls. Photo: HCSO.
Press release from the Humboldt County Sheriff’s Office:
On Dec. 30, 2025, around 10:30 p.m. Humboldt County Sheriff’s Deputies conducted a traffic stop near Salmon Creek Road on Northbound Highway 101 in Southern Humboldt County. During the stop, a Sheriff’s K9 was deployed to conduct a free air sniff of the vehicle’s exterior. The K9 alerted to the presence of illegal narcotics.
A subsequent search of the vehicle resulted in the discovery of a significant quantity of suspected controlled substances, including fentanyl, methamphetamine, cocaine, Xanax pills, MDMA and other prescription and illicit drugs. Deputies also located drug paraphernalia and items consistent with narcotics sales, including a digital scale.
The approximate seizure included the following:
- Fentanyl — 6.7 ounces and 35 suspected M30 fentanyl pills
- Cocaine — 18.58 grams
- Methamphetamine — 8 grams
- Xanax — 335 bars
- Methadone — One bottle of liquid methadone and 8 pills
- Lorazepam — 59 pills
- Oxycodone — 2 pills
- Suspected DMT — 4 grams
- Suspected PCP
- Numerous, as yet unidentified pills and pipes
The driver, identified as Michael Thurston, 47, of Rio Dell, was arrested, transported to the Humboldt County Correctional Facility and booked on the following charges:
- VC 14601.1(a) — Driving with a suspended or revoked license
- HS 11351 — Possession of a controlled substance for sale
- HS 11352(a) — Transportation or sale of a controlled substance
- HS 11375(b)(1) — Possession for sale or sale of a controlled substance
- HS 11375(b)(2) — Possession of a controlled substance
- HS 11350(a) — Possession of a narcotic controlled substance
- HS 11377(a) — Possession of a controlled substance
- HS 11364 — Possession of drug paraphernalia
- PC 182(a)(1) — Conspiracy to commit a crime
The passenger, identified as Tinisha Smith, 30, of Fortuna, was arrested, transported to the Humboldt County Correctional Facility and booked on the following charges:
- HS 11351 — Possession of a controlled substance for sale
- HS 11352(a) — Transportation or sale of a controlled substance
- HS 11375(b)(1) — Possession for sale or sale of a controlled substance
- HS 11375(b)(2) — Possession of a controlled substance
- HS 11350(a) — Possession of a narcotic controlled substance
- HS 11377(a) — Possession of a controlled substance
- HS 11364(a) — Possession of drug paraphernalia
- PC 182(a)(1) — Conspiracy to commit a crime
The Humboldt County Sheriff’s Office remains committed to protecting the safety and wellbeing of our communities by actively investigating and disrupting the transportation and distribution of dangerous drugs.
Anyone with information about this case or related criminal activity is encouraged to call the Humboldt County Sheriff’s Office at (707) 445-7251 or the Sheriff’s Office Crime Tip line at (707) 268-2539.
Recreational Dungeness Crab Fishing Now Open to Entire Humboldt Coast; Commercial Season Set to Open Jan. 15, Pending Domoic Acid Test Results
LoCO Staff / Wednesday, Dec. 31, 2025 @ 10:37 a.m. / Fish
Look at that tasty little guy! | Photo: CDFW
###
Press release from the California Department of Fish and Wildlife:
The last area of the recreational Dungeness crab fishery in Humboldt County opened today after being delayed due to elevated levels of domoic acid.
State health agencies determined that Dungeness crab in waters from the southern boundary of the Reading Rock Marine Protected Areas (41° 17.6’ N. latitude) to Cape Mendocino (40° 10.0’ N. latitude) can open. While the area is open to fishing, the California Department of Public Health (CDPH) issued a health advisory to not eat crab viscera (also known as guts) and to clean crab prior to cooking.
Following the recommendation from state health agencies, California Department of Fish and Wildlife (CDFW) Acting Director Valerie Termini declared the recreational Dungeness crab fishery open in the remaining delayed area of Humboldt County.
Due to the potential for whales in this area to become entangled in trap buoy lines, Dungeness crab may currently only be taken with hoop nets, crab snares, or by hand in accordance with the declared trap prohibition in RAMP Fishing Zone 1. Effective 8:01 a.m., Jan. 2, 2026, crab trap restrictions in this area will be lifted and all recreational gear types may be used statewide.
After being delayed due to entanglement risk, the commercial Dungeness crab fishery in the Central Management Area (Sonoma/Mendocino County line (38°46.125’ N. latitude) to Point Conception (34°27’ N. latitude)) will open on Jan. 5, 2026, at 12:01 a.m., under a 40% trap reduction. The trap reduction is expected to reduce entanglement risk for humpback whales by decreasing the number of vertical lines attached to traps in the water. The Dungeness crab season in the Northern Management Area (California/Oregon border (42° N. latitude) to the Sonoma/Mendocino County line) remains delayed because of the inability to conduct meat quality testing due to elevated levels of domoic acid. Pending results of ongoing domoic acid testing, the season will open on Jan. 15, 2026, at 12:01 a.m., under a 15% trap reduction.
For more information related to the risk assessment process, please visit CDFW’s Whale Safe Fisheries page. For more information on the Dungeness crab fishery, please visit CDFW’s Invertebrates of Interest: Crabs page.
For the latest information on domoic acid, health advisories and season closures, please see the following:
- CDFW:
Fishery closure information and health advisories page- Domoic Acid Fishery Closure Information Line: (831) 649-2883
CDPH:
- Domoic Acid results website (subsection Analytical Data – Crabs)
- Shellfish advisories page for latest consumption warnings
- Biotoxin information Line: (510) 412-4643 or (800) 553-4133
Why Aren’t There Buses to Bayside, or on Sundays?
Dezmond Remington / Wednesday, Dec. 31, 2025 @ 7:32 a.m. / Transportation
An HTA bus.
There are around nine miles between Arcata and Eureka, and there’s a lot of highway beyond both. For people without a car or with disabilities, covering the distances between Humboldt’s far-flung towns can be an insurmountable task without public transportation.
At recent public meetings around the county, the floor was open to members of the public who had “unmet transit needs” to share with local policymakers, who then passed them on to the Humboldt County Association of Governments (HCAOG). None of the Humboldt Transit Authority’s (HTA) buses run on Sundays and none of the Arcata & Mad River Transit System’s make it out to Bayside, two inconveniences that affected many of the commenters at Arcata’s unmet needs hearing on Nov. 19.
So why don’t they? — a simple question with several answers.
HCAOG’s associate regional planner Stephen Luther told the Outpost in an interview that they’d looked into Bayside service after many requests from community members, digging into census tract and transportation data. According to the 2020 census, there are roughly 1,800 residents in Bayside; six of them took the bus to work. HCAOG concluded that it wasn’t feasible because its population density isn’t high enough to justify the cost. Stops on the Red and Orange routes near the Murphy’s in Sunny Brae average around 30 people daily getting on and off there; Luther estimated adding stops deeper into Bayside would increase that by single digits.
“In terms of regular commuters that would be commuting into Arcata,” Luther said, “It was pretty low.”
According to last year’s unmet needs summary, buses used to run to Bayside “some time ago,” but that ended because so few people used it. HCAOG’s staff asked HTA if they could extend the Red line down Old Arcata Road to Bayside Corners; HTA said it’d add 8 minutes to the loop and couldn’t be done. In 2016, HTA added bus service down Old Arcata Road. Within two years, it was discontinued for the same reason.
Buses may one day run again to Bayside when the Roger’s Garage low-income housing project is constructed, according to the summary. But for the time being, it’s simply too expensive.
The same goes for Sunday bus routes. The big number: it’d cost about $600,000 annually to fund the route on Highway 101 called the Redwood Transit System (RTS), $200,000 from operating costs, like maintenance and fuel, and the rest from the five new people HTA would have to hire to keep operations running another day of the week.
HTA used to run buses on Sundays, but declining use during the pandemic killed it.
An estimated 237 people would use the service every Sunday. With the standard $2 rider fare, that means it’d run HTA about $15 every time someone rode the bus (what HTA calls their “operating subsidy”). It’d put that program deep in the red.
HTA’s deputy general manager Katie Collender told the Outpost they’re looking for an operating subsidy closer to $3 a rider.
Consultants for HTA also recommended that if RTS Sunday service started, the intra-city bus routes should also run on Sunday. Funding that would be another huge expense HTA can’t meet: $95,000 for Eureka and another $67,000 for Arcata (even when only running the Orange route).
“Bottom line and big picture, we’d love to have Sunday service,” Luther said. “We recognize it as an unmet need that does need to be filled. There are a lot of people that comment on this process that need the bus to get to work on Sundays. Who maybe work later in the evenings at a restaurant and rely on the bus to get home, but it doesn’t run late enough in the night. So there are many of these transit needs that we hear, year after year, that are just super challenging to implement.”
He said there was a “tension” between bus coverage and bus frequency; it’s expensive to add both at the same time.
“You really can’t have everything,” Luther continued a few minutes later. “We have a limited amount of funding. HTA does everything they can to get as many dollars as they can, to make it stretch as far as they can … If HTA can start a service and operate it, they’re going to.”
California’s Budget Outlook Is Grim. Here’s What You Need to Know
Yue Stella Yu / Wednesday, Dec. 31, 2025 @ 7 a.m. / Sacramento
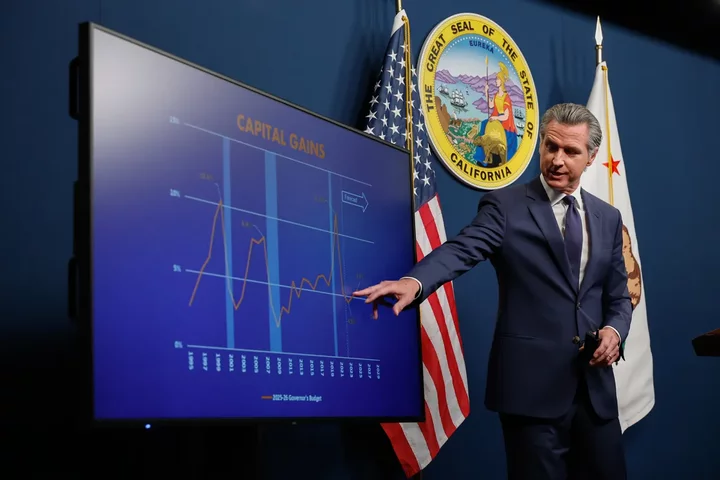
Gov. Gavin Newsom releases his revised 2025-26 budget proposal in Sacramento on May 14, 2025. Photo by Fred Greaves for CalMatters
###
This story was originally published by CalMatters. Sign up for their newsletters.
###
Gov. Gavin Newsom opened this year with a rosy forecast: Buoyed by $17 billion more in revenue than previously planned, the state would have a modest surplus of $363 million for fiscal year 2025-26, he told reporters in January.
But life turns on a dime.
The January wildfires that ripped through Los Angeles forced the state to spend billions in disaster aid and delay tax filings for LA residents. The cost of Medi-Cal, the state-run health insurance program for low-income residents, ballooned to $6 billion more than anticipated. President Donald Trump’s on-again-off-again tariff policies rocked the stock market, which California heavily relies on for tax revenue. And the state lodged a flurry of lawsuits against the Trump administration over its threat to withhold federal funding for food assistance, disaster recovery and other grants.
By May, Newsom no longer predicted a modest surplus, but a $12 billion deficit.
To plug the hole, Newsom initially proposed drastic cuts to Medi-Cal. But the final budget he negotiated with state lawmakers depended largely on internal borrowing, dipping into the state’s reserves and freezing Medi-Cal enrollment for undocumented immigrants to avoid deep cuts to other social services.
While Democratic leaders largely blamed the Trump administration for California’s budget problem, the volatility of state revenues is not new. California highly depends on taxing the income and capital gains of high earners, whose fortune is often at the mercy of the stock market. In 2022, the state saw a nearly $100 billion surplus, followed by a projected $56 billion deficit over the next two years.
2026 outlook
The deficit is projected to reach nearly $18 billion next year, mostly because the state is expected to spend so much money that it would offset, if not eclipse, the strong tax revenues driven by an AI boom, said the nonpartisan Legislative Analyst’s Office in its fiscal outlook last month.
If the estimate holds, it’ll be the fourth year in a row in Newsom’s tenure that California faces a deficit despite revenue growth.
Worse yet, the structural deficit could reach $35 billion annually by fiscal year 2027-28, the LAO said.
California is facing $6 billion in extra spending next year, including at least $1.3 billion because the state must now pay more to cover Medi-Cal benefits under Trump’s budget bill. The state also stands to lose more housing and homelessness funding from the federal government.
How can legislators fix it? The options are stretching thin, as the state already took one-time measures to balance the books. The LAO notes that solving an ongoing structural budget problem requires either finding more sustainable revenue streams, or making serious cuts, or both.